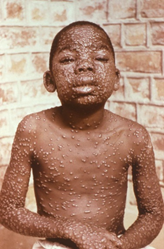
Figure 1. A young boy with smallpox. Source: CDC Public Health Image Library
At the end of this lesson, the student should be able to:
Disclaimer: All information in this case study is factually accurate and is based on actual events that occurred in the fall of 2001.
September 18, 2001. The country, still reeling from the 9/11 terrorist attacks, was just starting to understand the new normal when another attack occurred. The events of September 11, 2001 had a profound impact on our national consciousness and have become the ubiquitous example of modern terrorism. The next attack occurred seven days later and most people, unless they were directly affected by it, will likely not even remember it. A yet unknown person mailed a letter from a small post office in Trenton, NJ. This letter was later found to contain spores of the deadly bacteria anthrax. The envelope was sent to the offices of American Media Inc., the parent company for the Sun and National Enquirer tabloid magazines. The first report of illness occurred when Bob Stevens, a 63-year-old photo editor who worked in the office, started to experience flu-like symptoms. Investigators believe that he was exposed to the deadly toxin from the letter. Stevens was admitted to a Florida hospital on October 4, 2001 and the staff eventually identified that anthrax was the cause of the illness. A course of powerful antibiotics was initiated but it was too late and on October 5, Stevens died. Law enforcement agencies started to investigate immediately, but the source of the anthrax in the American Media Inc. offices was not identified until October 8. Anthrax poisoning was not identified in any other American Media employees.
On October 9, more anthrax-laced letters were posted from the same New Jersey post office. The FBI opened an investigation into these events the same day. On October 12, an employee who worked in NBC’s New York offices tested positive for anthrax poisoning. On October 15, Senate Majority Leader Tom Daschle told members of the media that anthrax spores were found in his office. On October 18, a CBS employee and a New Jersey postal worker tested positive for anthrax poisoning. On October 23, two postal workers from a Washington, DC postal facility were confirmed to have died from anthrax poisoning. On October 28, a New Jersey person became the 15th confirmed case of anthrax poisoning. Contaminated letters were also sent to NBC anchor Tom Brokaw, Senator Patrick Leahy, and the New York post offices. By the end of November 2001, there were 22 known cases of anthrax toxicity with five deaths. The contaminated letters stopped arriving just as suddenly as they began. The FBI and allied law enforcement agencies conducted an exhaustive investigation but no arrests wherever made.1,2
Etiological hazards, also known as biological agents, are microorganisms that can cause illness and disease. These microorganisms occur naturally throughout the environment and while some are normal and necessary for life, others cause illnesses which can range from innocuous to deadly. There are naturally occurring outbreaks of bacterial and viral illnesses that can cause significant public health problems. This includes illnesses like influenza, which according to CDC estimates, has resulted in between nine million and 45 million illnesses, between 140,000 and 810,000 hospitalizations, and between 12,000 and 61,000 deaths annually since 2010.3 While naturally occurring epidemics and pandemics are problematic and dangerous, they do not often involve direct response from public safety responders and hazardous materials teams. However, some biological agents can be weaponized. These agents are designed to cause illness, death, and panic throughout entire communities and populations. Biological agents have been used as weapons of war and terrorism throughout history. In the Middle Ages the corpses of plague victims were catapulted over castle walls to spread infection throughout otherwise fortified positions. There are various reports of British and early American colonists intentionally giving blankets infected with smallpox to Native Americans throughout the 1700 and 1800s. Smallpox was new to this population and was absolutely devastating, killing as many as 90 percent of those who were infected. During World War I, Germany developed a variety of weapons using anthrax glanders and cholera. Additionally, it is alleged that the Germans attempted to spark a plague outbreak in St. Petersburg. Throughout World War II, the Japanese operated a covert biological weapons development facility in Manchuria. There they exposed more than 3,000 prisoners to a variety of diseases including plague, anthrax, and syphilis in an attempt to weaponize the agents. Today the use of biological weapons is prohibited by Rule 73 of the Geneva Convention. While many nations maintain stockpiles of dangerous viruses and bacteria for research purposes their use in weapons is explicitly prohibited by international law. Current biological weapons threats come from terrorist groups and rogue nation-states. A biological weapons attack will likely be far more complicated than typical hazardous materials incidents where a product has to be identified, a leak stopped, and a site has to be cleaned up. Public safety personnel and hazardous materials team members will have to work with public health groups like the Centers for Disease Control (CDC) to identify, quarantine, and treat people who have been or potentially have been exposed. This course will help prepare responders by identifying the different types of biological agents that may be encountered during a Hazmat incident, describe how to identify the presence of different types of biological agents, discuss the different types of personal protective equipment (PPE) and resources that may be needed based on the identified biological agent, and by reviewing decontamination procedures for various biological agents.
The biological agents that have the potential to be weaponized and may be encountered during a hazardous materials incident are divided into three categories. They are viruses, bacteria, and biological toxins. Viruses reproduce in the living cells of host organisms. Antibiotics are an ineffective treatment modality for managing viral infections. Smallpox is caused by a virus. Bacteria are single-celled organisms that can invade tissues and produce toxins. Anthrax is the result of bacterial infection. Rickettsia are specialized bacteria spread by fleas, ticks, and lice. They are smaller than most bacteria but are larger than viruses. Plague and the typhus group of fevers are common rickettsias. Biological toxins are hazardous substances produced by living things such as microorganisms, animals, insects, and/or plants that can cause illness or injury when absorbed, injected, or inhaled by humans. Ricin is a biological toxin that has been synthesized and weaponized in the past.
Biological weapons are designed to cause widespread death, illness, and panic. They will produce lethal or incapacitating effects at achievable doses. In the majority of cases biological weapons are delivered through aerosolization where the particles are dispersed through the air and then inhaled by the victims. The route of dermal absorption where the toxin is absorbed through skin contact is also possible but much less likely. Aerosols are used because they can be easily spread over distance and infect large groups of people. Additionally, they tend be colorless and odorless making them incredibly difficult to detect.4 Biological weapons can be dispersed using rudimentary and unsophisticated delivery devices which increases their popularity among terrorist groups. Prior to the Gulf War, in 1988 and again in 1991, Iraq is reported to have used commercially available agricultural sprayers that were modified to disperse biological agents against populations of civilian Kurds. Additionally, disease vectors have been used to spread biological agents. During WWII Japan cultivated plague-carrying fleas which were then dropped onto several Chinese cities causing widespread bubonic plague outbreaks.5 Unlike other chemical agents, biological agents may have limited stability in the environment. Some of the agents are sensitive to light and temperature. Others can only survive outside of a host organism for a limited amount of time. The persistence and stability of each agent will have a significant impact on their spread and duration in an exposed population.
The rest of this course will focus on CDC Category A Biological Agents. These agents were given this designation due to their ability to cause the gravest harm to an unprotected population. This is based upon the agent’s potential to cause disease, death, and disability, the ability to cause panic within a population, the ease of dispersal through aerosolization, and the availability of effective therapies.6 The biological agents that will be described include smallpox, anthrax, plague, botulism, tularemia, and viral hemorrhagic fever.
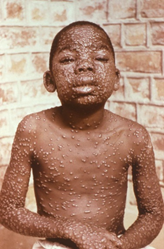
Figure 1. A young boy with smallpox. Source: CDC Public Health Image Library
Smallpox is a viral illness caused by the orthopox virus. There are two strains: variola major and the milder variola minor. There is a vaccine available and the disease is considered globally eradicated in the natural environment. However, potential weaponization remains a threat due to aerosol infectivity, the potential for large-scale production, and a growing immunologically naive population (anti-vaccinators). Smallpox presents with non-specific flu-like symptoms and eventually develops with a widespread blistering rash from which its name is derived.
In 1980 the World Health Organization (WHO) declared endemic smallpox eradicated. There are two WHO approved virus repositories that were known to have smallpox virus. They are the CDC headquarters in Atlanta and the Institute for Viral Preparedness in Moscow. In 1996 the WHO recommended that these viral stockpiles be destroyed by 1999. In the United States the federal government delayed its destruction due to the need for further study and research. Today, it is unknown if these repositories still exist.7
Smallpox has a long history of use as a biological weapon. It has been reported that until the 18th century the British Army used it against Native Americans.8 Japan attempted to produce large quantities of the virus and considered its use in WWII. There are additional reports indicating that the Soviet Union produced and stockpiled large quantities of smallpox during the Cold War. It is unknown if that cache of viruses still exists.9 Widespread but unvalidated rumors indicate that a large quantity of Soviet manufactured weapons of mass destruction including biological weapons have become available on the black market and are being illicitly traded among terrorist organizations. This may be a primary source for the smallpox virus that threatens the modern world.
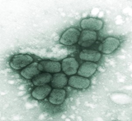
Figure 2. Smallpox virus viewed through an electron microscope. Source: CDC Public Health Image Library
In the early 1980s the American civilian smallpox vaccination program was discontinued due to global eradication of the virus. Additionally, the military ended its vaccine program in 1989. In 2002 and 2003 selected military and civilian populations were vaccinated as a precaution. Today, the loss of herd immunity would significantly increase the number of people who became ill and would die should a smallpox outbreak occur. The mortality associated with smallpox infection depends on the strain of the virus that is present. Among patients infected with variola minor, the less severe strain, the mortality is only one percent among unvaccinated populations. If the infection stems from variola major, the mortality rate among vaccinated populations is between three and 30 percent among unvaccinated individuals. Hemorrhagic smallpox, the most severe form of variola major infections, occurring in two percent of all smallpox cases, could lead to 100 percent mortality among all population
Figure 3. Anthrax spores. Source: CDC Public Health Image Library
Anthrax is caused by the bacterial spore bacillus anthracis. It is naturally occurring and infection can occur after contact with infected animals or animal products. In humans the disease is contracted through scratches, abrasions, other open wounds, via inhalation or through the ingestion of insufficiently cooked meat. It is a gram-positive, spore-forming rod. Anthrax is a popular agent of bio terrorism because the spores are highly stable and can remain viable in soil and water for years, the spores are resistant to sunlight, heat, and disinfectants, and they are easily lab produced. The greatest terrorist threat is inhalation after aerosol dissemination of spores. Anthrax was first weaponized by the United States in the 1950s and 1960s. It was also developed and used by other countries including the USSR, Japan, and Iraq. It was deployed in a terrorist attack against the US in 2001 which was described in the case study.
Plague is caused by yersinia pestis which is a rickettsia, rod-shaped, non-motile, non-sporulating, gram-negative bacterium. It is zoonotic, meaning that it is borne by animals. Plague is primarily found on rodents such as mice, rats, and ground squirrels. It is spread to humans by the bites of fleas that live on the animals. The infection results in bubonic plague which can progress to septicemic and or pneumonic form. Pneumonic plague will be the dominant type of infection after an aerosol dispersion of the weaponized form. Plague bacteria remains viable in dry sputum, flea feces, and cadavers for extended periods of time and it can be persistent in water, moist soil, and grain. At cold temperatures (near freezing) it can remain alive for months to years. However, it is killed within minutes of exposure to temperatures at 55 degrees Celsius or higher and within several hours of exposure to sunlight.10 All human populations are susceptible. For those individuals who survive the infection there is a brief period of immunity after recovery. The mortality associated with untreated bubonic plague is approximately 60 percent and it increases to almost 100 percent for pneumonic plague when it is untreated.11 Since the 1950s there have been seven cases of pneumonic plague identified in the United States and four (57 percent) of the patients died despite receiving treatment. There has been an ongoing outbreak of bubonic plague in Madagascar since 1989 and modern treatment modalities have been shown to reduce the mortality rate to less than five percent.12
The plague has been weaponized by the US, Japan, and Russia. There are known to be reliable and effective methods of aerosolizing the organism. In 1995, Larry Wayne Harris was arrested and accused of a terrorist plot in Ohio after illicitly procuring plague cultures. According to news reports, Harris, a member of the Aryan Nation terrorist group, posed as a scientist and ordered the samples from the American Type Culture Collection in Rockville, Maryland. The staff at the Maryland lab became suspicious and alerted law enforcement. The samples, which were mostly inert bacteria, were found in Harris’s car and firearms, bomb-making materials, and white supremacist literature were discovered at his residence. Eventually Harris was convicted of fraud and served 18 months of probation. The case did, however, prompt Congress to enact legislation that now requires CDC registration when disease-causing organisms like the plague are being shipped.13
Botulism is a group of seven related neurotoxins produced by the anaerobic motile, spore-forming, gram-positive rod Clostridium botulinum. Botulism toxins are some of the most toxic compounds in the world. At doses of 0.001 microgram/kg of body weight they are known to kill 50 percent of study animals.14 In the medical environment they have a variety of therapeutic and cosmetic uses. The popular Botox injections, used to treat skin wrinkles, are a highly diluted form of botulism toxin. Botulism is also caused through the ingestion of improperly prepared canned foods and has led to many deaths. Botulism spores germinate in vegetative bacteria that produce toxins during anaerobic incubation. Industrial scale fermentation can produce large quantities of toxins for use as biological warfare agents.15 These toxins could be delivered as an aerosol and used to contaminate food and water supplies, making it a deadly and effective weapon. Botulism was first weaponized by the US prior to 1969. In 1995 it is alleged that Iraq filled and deployed over 100 munitions with nearly 10,000 liters of botulinum toxin. In Japan, the Aum Shinrikyo cult weaponized and attempted to disseminate botulinum toxin on numerous occasions.16
Tularemia, also known as rabbit fever or deer fly fever, is caused by the Francisella tularensis bacteria. It is a naturally occurring zoonotic disease that humans typically acquire after skin or mucous membrane make contact with tissue or bodily fluids from infected animals. It is also spread by the bites of infected ticks, deer flies, and mosquitoes. Additionally, tularemia can be spread through the inhalation of contaminated dusts or the ingestion of contaminated food and water. The bacteria are viable for weeks in water, soil, and animal tissues. Fortunately, it is easily destroyed with heat and disinfectants. Inhalation of the bacteria leads to pneumonic tularemia which is often fatal when untreated. In the early 1900s tularemia was first identified in the United States after an outbreak in San Francisco. The bacteria were first weaponized by the Unites States and the Soviet Union in the 1950’s and 1960s in both dry and wet delivery forms. There are additional unconfirmed reports of other countries producing weapons using tularemia.17
Figure 4. The Ebola virus. Source: CDC Public Health Image Library
Viral hemorrhagic fevers are a wide group of illness caused by four different viral families. The most well-known of which is the Ebola virus. These viruses are easily transmitted through a variety of routes including aerosol inhalation and are often fatal. While there is no current evidence of their use in a weaponized form the CDC includes them as a Class A biological agent because of their potential for aerosol dissemination and the catastrophic harm that they could cause.18
An attack using biological weapons may go undetected for hours, days, or possibly even weeks. Unlike conventional weapons, biological weapons do not present with any evidence that is immediately visible to victims, bystanders, and/or responders. According to the Department of Homeland Security (DHS), the detection of a biological attack will most likely occur when local healthcare providers identify unusual patterns of illness in their communities.19 Once a pattern emerges, samples from the victims will then be sent to specialized laboratories where analysis and testing will be used to confirm the presence of the suspected agent. After that, epidemiologists and public health experts will trace the path of infection or contamination back to the initial patient, disease vector, vehicle (food or water), or other point of origin.20 There are some early warning monitoring systems that are used in an attempt to detect the presence of biological agents in the air but their efficacy is limited at best.
The dissemination of a biological agent may occur in a number of different ways. Some agents may be produced as an aerosol suspension where they are cultured and processed to proper size to maximize human infections while maintaining stability and pathogenicity.21 The agent will then be spread using commercial sprayers or other similar devices. This type of attack will likely occur outdoors in a highly populated area, in the ventilation systems of commercial buildings, or in a closed compartment such as an aircraft or subway. Food supplies, especially ready-to-eat foods, may be intentionally contaminated with pathogens or toxins. In 1984, members of an extremist cult in Oregon infected 751 people with salmonella by placing bacterial cultures in restaurant salad bars. While many people were hospitalized no deaths were attributed to this attack. Intentional contamination could potentially also impact water supplies but for biological agents the threat is relatively low. The dilution, filtration, and chlorination systems that are part of water distribution infrastructure will destroy the majority of disease-causing organisms.22 Human carriers may be used to spread transmissible agents throughout communities. Infected animals or insect carriers could also be used as disease vectors to intentionally spread pathogens. Finally, agents can be physically distributed using US mail or other means.23
Public safety responders should be aware of the general signs and symptoms of illness caused by biological agents. Smallpox is caused by a virus which obviously cannot be seen. As with the majority of biological agents an outbreak will not be identified until people start to get sick. The patients will initially present to primary care and emergency departments. The confirmation of the presence of smallpox will be made by CDC laboratories after medical providers rule out more common illness such as chickenpox.24 The clinical presentation of smallpox occurs after an incubation period of seven to 17 days (average is 12 days). The acute clinical manifestations after the incubation period include malaise, fever, rigors (chills with shivering and shaking), vomiting, headache, and backache. Approximately 10 percent of patients exhibit an erythematous rash (generalized skin redness) during this phase of the illness. Two to three days later an exanthem (widespread rash) appears on the patient’s face, hands, and forearms. After that the rash spreads to the patient’s lower extremities and trunk. One of the main differences between the presentation of smallpox and chickenpox is the distribution of the blistering rash. In the majority of cases the rash associated with chickenpox is centripetal, meaning that it is most apparent on the trunk and is seldom seen on the palms of hands and soles of feet. The lesions caused by smallpox are centrifugal, are most apparent on the extremities and face, and commonly found on the patient’s palms and soles. The lesions progress from flat macules to raised papules and eventually to pustular vesicles (pus-filled blisters). The lesions tend to be most apparent on the patient’s extremities and face. Eight to 14 days after they appear, the pustules form scabs which eventually leave depressed scars. Patients with smallpox should be considered infectious and quarantined until all scabs have dried up and fallen off.
The bacterial spores that cause anthrax could be placed in the mail (i.e. the 2001 attack) and food and water might also be contaminated. The aerosol release from a vehicle or fixed structure is also possible. A small amount of anthrax spores could infect a large number of people.25 The presence of anthrax could be detected in three ways. The first is through established CDC monitoring systems that are deployed nationwide. If those systems fail to detect its presence, then patterns of unusual illness would be identified by emergency room personnel and other healthcare providers. The third way is a five-step process that has been developed for testing suspicious powder reported by concerned citizens. This test was developed in response to the widespread calls for service involving suspicious powders after the 2001 attacks. This field test has been validated in the laboratory setting with 99 percent confidence, meaning that if all five steps are negative, there is a 99 percent chance that the powder does not contain anthrax spores or other harmful biological agents.26 Regardless of the results of the testing, it is recommended that samples are sent to a lab to substantiate the findings. The equipment needed to complete the testing includes two 3 mL glass or borosilicate vials, pH paper test strips with a comparison chart, protein test strips with a comparison chart, a small disposable scoop or spatula, distilled water, a magnifying glass, and a flashlight. Once all of the equipment is prepared the first step is to collect two samples using the scoop and place them in the glass vials with the lid fastened tightly. The first sample should contain a volume equivalent to a restaurant sugar packet and should be secured for laboratory analysis. The second sample is for field testing and should be a volume similar to the size of a pea or corn kernel. The second step is to take the field-testing sample and shake it vigorously. After shaking the sample should be observed with the magnifying glass. If the sample contains a biological agent a fine cloud of small particulate will hang in the air above the sample for several seconds. If all material immediately falls back to the bottom of the vial after shaking, the test is negative and it is unlikely that it contains any biological agents. Next, 2 mL of distilled water should be added to the sample and it should be shaken for 15 seconds. The test is positive if the sample mixes with the water but does not dissolve and the liquid remains cloudy or turbid. The test is negative if the sample dissolves in the water and becomes clear without larger particles settling to the bottom. The fourth step is to test the solution in the vial with a pH test strip. If the solution’s pH is between five and nine, then it is positive. If the pH is less than five or greater than nine, it is negative. The fifth and final step is to test the solution in the vial with a protein test strip. The test is positive if protein is present and negative if protein is not present.27 The flashlight is used to illuminate the sample and ensure appropriate visualization during testing. Take note, this description of the testing process is not intended to provide credentialing to perform the procedure. Responders who will be expected to perform this test in the field should receive training and certification from accredited hazardous materials training agencies.
Once anthrax is suspected it should be confirmed with laboratory testing.28 When a person is exposed to anthrax there is an incubation period of one to six days before the first signs and symptoms of illness appear. In most cases the initial clinical presentation is non-specific including fever, malaise, and fatigue. A non-productive cough and mild chest discomfort may be present. Typically, after the initial illness there is a period of improvement lasting two to three days, which is then followed by the abrupt development of severe respiratory distress with diaphoresis and cyanosis. After the onset of dyspnea, septicemia, shock, and death follow within 24 to 36 hours.29 If patients who are exposed to inhalation anthrax are not treated until they present symptoms of the disease it is often fatal.30
Plague appears in three forms. They are bubonic, septicemic, and pneumonic. Identification of a weaponized plague attack will be based on clinical suspicion when there is the sudden presentation of large numbers of previously healthy patients with the same symptoms including rapidly progressing pneumonia with hemoptysis (bloody sputum).31 Bubonic plague is typically transmitted by the fleas that live on infected rats and mice. Bubonic plague has am incubation period of two to 10 days, after which the patient will begin to experience fevers, malaise, headaches, muscle aches, and sometimes gastrointestinal distress with nausea and vomiting. Additionally, the patient’s lymph nodes in the femoral and inguinal areas will become inflamed and painful. These are called buboes and is where the disease’s name is derived from. Pus-filled skin lesions are also common. The largest outbreak of bubonic plague occurred in Europe in the Middle Ages and is widely known as the Black Death. The outbreak lasted 275 years and killed approximately one-third of the population of the entire continent. Septicemic plague can occur as a result of bubonic plague or on its own. Patients with septicemic plague will present with primary sepsis and shock. They may also exhibit necrotic appendages, gangrene, and disseminated intravascular coagulopathy. Pneumonic plague is an infection of the lungs due to the inhalation of plague organisms or secondary infection after bubonic plague. A biological weapons attack using plague would most likely employ aerosolization which tends to cause pneumonic plague. For pneumonic plague there is an incubation period of one to six days followed by the presentation of symptoms with high fever, chills, headache, malaise, and body aches. Gastrointestinal distress with nausea, vomiting, and diarrhea is common. Within 24 hours a cough with bloody sputum develops in most cases. When a chest X-ray is performed the majority of patients will have bilateral infiltrates. A lung infiltrate occurs when a substance such as blood or pus collects in the lung parenchyma. This is a hallmark of pneumonia and can significantly impair the respiratory process. As the disease progresses patients will experience respiratory distress, respiratory failure, and then circulatory collapse.
An attack involving botulism will become apparent with a sudden epidemic of afebrile patients with progressive, symmetrical, descending paralysis.32 The early symptoms are the result of cranial nerve impairment. When the toxin is delivered through inhalation, symptoms usually occur 12 to 36 hours after exposure. The presentation is variable and is dependent on the amount of inhaled toxin. Patients suffering from botulism are afebrile, alert, oriented, and lack fasciculations. Fasciculations are involuntary muscle twitches and are often associated with the toxicity resulting from exposure to nerve agents such as VX or sarin gas. Additionally, patients with botulism will also experience symptoms including blurred vision, mydriasis (dilation of pupils), photophobia (visual discomfort caused by light), diplopia (double vision), and ptosis (drooping of the upper eyelid). There can be upper airway insufficiency due to weak or paralyzed oropharyngeal musculature. As the disease progresses Ps and Ds appear and/or become more pronounced. The Ps are ptosis, paresis (partial paralysis), and paralysis. The Ds are descending, diplopia, dysphonia (difficulty speaking due to weak oropharyngeal musculature), dysarthria (difficulty articulating), dysphagia (difficulty swallowing), and death.33 In severe cases patients will require extended periods of ventilatory support due to associated respiratory failure.
If tularemia was to be weaponized the most likely route of delivery would be through aerosolization which would cause typhoidal tularemia. The patient’s symptoms would manifest after an average incubation period of three to five days. The symptoms include fever, weight loss, and prostration.34 Pneumonia may be present and patients will often experience dyspnea, chest pain, and cough. Without treatment typhoidal tularemia has an approximate 35 percent rate of mortality. Tularemia is diagnosed through culturing blood, sputum, and other bodily fluids.
Viral hemorrhagic fever (VHF) is a general term for a diverse group of illnesses caused by ribonucleic acid viruses from four different viral families. They are the Arenaviridae, Bunyaviridae, Filoviridae, and Flaviviridae viruses. The Filoviridae family includes the Ebola and Marburg viruses. Flaviviridae encompasses the dengue and yellow fever viruses. Bunyaviridae includes the hantaviruses and the Crimean-Congo hemorrhagic fever. Arenaviridae includes the etiological agents of Argentinian, Bolivian, Brazilian, and Venezuelan hemorrhagic fevers.35 In general these viruses are highly contagious and can be spread through respiratory droplet inhalation. The Ebola virus was first identified in Sudan and Zaire in the 1970s. A large outbreak occurred in Zaire in 1995 when one infected person spread the disease to 315 more. The strains of Ebola that are present throughout Africa cause severe illness and death. The symptoms of VHF include fever, body aches, and prostration. Early in the disease process patients will often experience petechial hemorrhage (bruising that appears spontaneously), flushing, and mild hypotension. As the disease progresses patients develop shock, mucous membrane hemorrhage, pulmonary hemorrhage, and renal failure.26 On August 1, 2018, the Ministry of Health in the Democratic Republic of Congo (DRC) first reported an outbreak of Ebola. The outbreak occurred in an area of the country where there is frequent armed conflict, endemic distrust of government/outside agencies, and little infrastructure which has complicated both the national and international public health response. On March 24, 2019, the CDC announced the outbreak was ongoing and had surpassed 1,000 cases. 37 On July 17, the World Health Organization (WHO) declared the outbreak a public health emergency of international concern citing its duration and potential for cross-border spreading.38 As of this publication there are at least 3,000 confirmed cases and 2,000 deaths making it the second largest recorded outbreak of Ebola in the world. Any patient who has a fever and has traveled to Africa within the last 21 days should be considered a potential carrier of the Ebola virus. When EMS agencies respond to calls for service involving febrile patients the patient should be asked about his or her travel history while responders are standing off at a distance of six to eight feet. If he or she acknowledges recent travel to Africa or close contact with individuals who have traveled to Africa the crews must immediately retreat and prepare the appropriate PPE. This will be described in detail in the next section of the course.
An attack or outbreak of a biological agent will cause widespread illness and death throughout the affected community. Responders from local, regional, state, and often federal agencies, public health agencies, and law enforcement including the FBI will all be involved in the response. Incidents involving biological agents are extremely resource-intensive, costly, and time-consuming. It will also cause panic encompassing an even wider geographical area. This panic will have a significant impact on public safety resources and medical infrastructure. Medical centers, emergency rooms, and EMS agencies will be overwhelmed with patients who report illness but may or may not be infected with or exposed to the agent. Hazardous materials teams, fire departments, EMS agencies, and law enforcement agencies will be inundated with calls for service reporting suspected hazards. Following the 2001 anthrax attacks there was an overwhelming number of calls from citizens reporting suspicious white powder in public places. The vast majority of these calls were unfounded and involved dust, talcum powder, table salt, sugar, or other harmless powder but they all had to be investigated. The FBI reports that there were approximately 50,000 of these incidents by the end of 2002.39 There have also been intentional white powder hoaxes. In October 2008, 53 letters mailed from Amarillo, Texas to banks and government offices across the country contained threatening statements and white powder. Field testing at the sites quickly determined that the powder was inert and there was no hazardous condition but there was still a significant expenditure of resources and manpower.40 The previously described five-step process to determine the hazard associated with unknown powder was developed in response to these situations.
In 1999, the Strategic National Stockpile was established to increase preparedness and provide a cache of antibiotics, vaccines, chemical antidotes, antitoxins, and other critical medical supplies. This supply, now valued at over $7 billion, is deployed to covert facilities across the country and is set up in push packages that are strategically placed to be available anywhere in the country within 12 hours. The supplies are palletized and ready to be loaded onto trucks or aircraft and be delivered at a moment’s notice. The available inventory includes millions of doses of vaccines against bioterrorism agents like smallpox, antivirals in case of a deadly flu pandemic, medicines used to treat radiation sickness and burns, chemical agent antidotes, wound care supplies, IV fluids, and antibiotics.41 The repositories contain sufficient supplies and equipment to support the response to multiple large-scale incidents simultaneously. It is reported that there are 300 million smallpox treatment courses and enough anthrax vaccine to handle a three-city incident.42 In 2009, the strategic national stockpile released and deployed large quantities of its antiviral drugs Tamiflu and Relenza, PPE, and respiratory protection devices to help every US state respond to the H1N1 (swine flu) pandemic.
In addition to the stockpiled equipment and supplies, FEMA has disaster medical assistance teams (DMAT) available should an emergency exceed the scope of a community’s healthcare resources. There are 55 teams across the country comprised of doctors, nurses, paramedics, and other allied healthcare providers that are available to deploy to disaster sites. When a DMAT responds it will bring a mobile hospital with sufficient supplies and equipment to operate independently for a 72-hour period. Additional supplies and equipment can be pushed in behind the team if the operations will continue after the initial period. In situations where there are large numbers of deceased victims FEMA also maintains 11 disaster mortuary teams (DMORT) which are deployable to assist with the recovery, identification, and processing of deceased victims. These resources have been deployed for disasters such as Hurricanes Katrina and Sandy, the earthquake in Haiti, and the Joplin, Missouri tornado. These resources are available at any location in the country where they are needed and can be requested through standard PSAPS; however, the deployment of federal assets typically requires a federal emergency or disaster declaration.
If an incident involving biological agents occurs the CDC will respond as soon as it is identified. The CDC actions include coordinating through the EOC to communicate with the public, guiding healthcare providers, engaging its laboratory response network to test samples, deployment of field staff to evaluate the spread of the disease, and shipping out vaccines and other supplies from the Strategic National Stockpile.
A smallpox outbreak would be an international public health emergency. The CDC recommends droplet and airborne precautions be maintained for at least 17 days for all persons with contact with the index case (the first known patient to develop the disease). Quarantine for these individuals would be useful but difficult to maintain. For any individual who has had contact with a known case of smallpox a fever of 101 degrees or greater that manifests during the 17-day post-exposure period suggests development of the disease. Patients with smallpox remain contagious until all of the scabs have fallen off. All individuals and responders who are exposed to suspected cases of smallpox should be vaccinated or revaccinated within three days of exposure. However, once the rash develops the vaccine is ineffective.43 For responders and healthcare providers standard blood and body fluid precautions including disposable gowns and gloves, NIOSH certified N95 masks, and eye protection are the CDC recommended PPE. Additionally, hand washing with soap and water or hand sanitizer is a priority. Infected patients who have developed rashes and cannot be vaccinated should be managed with supportive care.
When anthrax is suspected or possible, level C Hazmat PPE is required. Level C PPE includes chemical resistant Tyvek or equivalent suits, air purifying respirators, goggles, two layers of gloves, and booties. Once properly dressed in level C PPE, responders should approach the suspect powder and perform the five-step process testing for the presence of biological agents. All testing should be performed in PPE where the powder was found to prevent further spread and contamination.
Any individuals who have come in contact with the powder must be decontaminated. The procedures for decontamination will be discussed in the following section. Once the individuals have been decontaminated only standard blood and fluid isolation precautions are needed. There is no evidence to indicate that inhalation anthrax is spread by contact with infected patients unless they are contaminated with spores. Exposed individuals should be prophylactically treated with antibiotics like Cipro. Individuals who become ill should be managed with supportive care.
If plague is suspected standard body substance isolation (BSI) precautions with strict respiratory and droplet precautions should be maintained. Patients will require 48 hours of antibiotic therapy in addition to standard supportive care. If zoonotic vectors are present, they need to be controlled as much as possible. Exterminators, animal control workers, and/or entomologists may be needed to assist in this process.
If botulism is suspected standard BSI precautions are required. There is no known person-to-person spread with inhalation botulism. Sick individuals should be administered botulinum antitoxins and provided with supportive care. Once the vector with which the botulism was delivered has been identified the source will have to be secured and destroyed and the affected area needs to be thoroughly decontaminated.
There is no known human-to-human spread of tularemia. Isolation and quarantine are not required.44 When patients are experiencing typhoidal tularemia or present with draining lesions, standard isolation precautions for blood and body fluids are appropriate. Any soiled clothing, bedding, and equipment must be thoroughly decontaminated. Heat and/or standard disinfectants are effective against tularemia.45 Patients with suspected tularemia should be treated with the antibiotics gentamycin, ciprofloxacin, or streptomycin. Individuals who have been exposed but are not sick may benefit from prophylactic courses of the antibiotics. There is a vaccine available but it may not be effective after the person has been exposed to the disease.
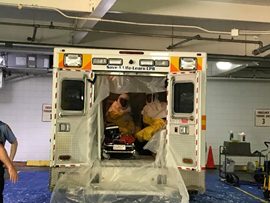
Figure 5. Pittsburgh EMS ECHO team. Training demonstration
Viral hemorrhagic fevers tend to be highly contagious. It is recommended that patients with known or suspected VHF should be isolated in individual, non-recirculated air, negative-pressure hospital rooms with adjoining anterooms for donning PPE, decontamination, and storage of laboratory specimens. Any person entering the room should have at least gloves and a gown on. Additionally, any person coming within three feet of the patient should also don surgical masks and eye protection. If the patient has or develops a prominent cough, vomiting, diarrhea, or hemorrhage, the PPE ensemble should be upgraded to include powered air purifying respirators or positive pressure supplied air systems like SCBA. If EMS providers are treating and transporting patients with known or suspected VHF, level B hazardous materials PPE with powered air purifying respirators or SCBA should be worn. When VHF patients must be transferred from one medical facility to another, transport teams that are specially trained and equipped to manage highly infectious patients should be utilized. One such team is the Pittsburgh EMS ECHO team, an all-hazards support team, whose primary mission as a regional and statewide asset is to respond to, isolate, treat, and transport any patients involved in a potential contagious or biological event. Any specimens collected for laboratory analysis must be double-bagged and the exterior of the outer bag must be decontaminated prior to transport.46 Patients with VHF should receive supportive care with special attention paid to limiting invasive procedures that may cause additional hemorrhage. The care will focus on providing fluid replacement therapy, supplemental oxygenation as needed, and using medication to support perfusion, reduce vomiting, and to manage fever and pain as well as treating other secondary infections. In December 2019, the FDA approved the first Ebola vaccine. The drug, named Ervebo, was developed by Merck, protects against the Zaire strain of Ebola, and is approved for adults over the age of 18.47 Additionally, there are a number of antiviral drugs that are being developed and deployed but there are none that are currently FDA approved. Throughout the current DRC Ebola outbreak the investigational antiviral drugs Regeneron and mAb114 have been used and substantially higher rates of survival have been observed.48
When biological agents are known or suspected, decontamination of civilians who have been exposed as well as responders will be a priority. There are agent specific recommendations that will be discussed later in this section. Additionally, responders should be aware of general hazardous material decontamination principles. If an attack occurs in a crowded public space or occupied structure mass decontamination may be the only viable option during the initial phases of the incident. Mass decontamination is utilized when there are large groups of civilians in a potentially contaminated environment who are ambulatory and need to be quickly decontaminated - prior to triage and transport to definitive care. This process is not considered equivalent to hazard-specific procedures but at times it may be the only feasible option. One way to complete mass decontamination is to place two fire engines parallel to one another approximately eight feet apart. Then, one or two ground ladders are placed across the span between the two trucks. Hand lines are then positioned on the ladders and fog streams at low to moderate pressure are directed at the ground. The contaminated individuals are then instructed to strip down to their underwear and walk through the water, washing off as much of the contaminated material as possible. If it is feasible, soap can be provided for the people to wash themselves with. When completing mass decontamination, the ambient temperature as well as the modesty of the individuals going through must be considered. Responders must be ready to provide warming blankets and towels as soon as everyone completes the decontamination process. All of the garments that are removed must be collected, bagged, and secured by responders wearing appropriate PPE. Finally, if it is possible, all of the water that is used in the decontamination process should be contained and retained because it is now contaminated with whatever material is present. It is understood that this may not be possible in some situations. Responders who are treating and transporting patients who have been decontaminated in this manner may want to consider continuing to wear PPE in case the process was insufficient. Receiving facilities should be given as much advance notice as possible because they may want to set up additional decontamination prior to entry into the facility. Responders should be decontaminated using product-specific best practices.

Figure 6. Pittsburgh EMS ECHO Team decontamination training
The current best practices for disinfection and sterilization when smallpox is suspected include the use of hospital grade disinfectant to cleanse all surfaces in patient care areas, all surfaces in ambulances, and all responders. There is no EPA-registered disinfectant approved to inactivate variola virus (the virus that causes smallpox). Since variola virus is similar to vaccinia virus (the virus used in the smallpox vaccine), any EPA-registered hospital disinfectant approved to inactivate vaccinia virus may be used to disinfect nonporous surfaces contaminated by variola virus. Follow the manufacturer’s recommendations for concentration, contact time, and care in handling. The nature and extent of surface contamination will dictate the level of disinfection.49 All contaminated and potentially contaminated laundry should be considered a vector of disease spread and handled accordingly. Additionally, enhanced waste management regulations using autoclaves and incinerations should also be used.
Anthrax spores are environmentally persistent, meaning that they can survive for extended periods of time. All contaminated areas must be disinfected with sporicidal agents, disinfectant strength iodine, or undiluted bleach. The recommended decontamination procedure for contaminated civilians is to have individuals remove all clothing and jewelry and then skin and hair should be washed with large quantities of water and mild liquid detergent. All of the removed garments and jewelry must be bagged and secured because they may contain anthrax spores.
Plague is decontaminated with hospital grade antibacterial disinfectant. Pest control and the eradication of zoonotic disease vectors will also be a primary goal when working to stop the spread of the disease.
Decontamination for botulism includes the removal of all clothing and jewelry and then washing with large quantities of liquid detergent. Responders and equipment should be decontaminated with dilute bleach solution. Additionally, sunlight inactivates the toxin within one to three hours.
Tularemia is easily destroyed with heat and hospital grade disinfectants. All responders and equipment that are potentially exposed should be deconned with disinfectant. Autoclaves and trash incineration should be used when appropriate and feasible.
When VHF is known or suspected an FDA approved antimicrobial product for non-enveloped viruses should be employed. A list of EPA registered products that are approved for use with the Ebola virus or other VHF-causing viruses is available here: https://www.epa.gov/sites/production/files/2018-01/documents/2018.10.01.listl_.pdf. All responders and non-porous surfaces should be cleaned thoroughly using one of these products. Materials that can absorb fluids such as linen, pillows, and mattresses should be disposed of and incinerated. The viruses that cause VHF can remain active in blood and bodily fluids after the patient’s death. Deceased victims should be sealed in fluid impervious bags and be promptly buried or cremated.
The anthrax mail attacks that occurred in the fall of 2001 killed five people and sickened 17 others. The victims that died all suffered from inhalation anthrax. More than 32,000 individuals were treated prophylactically with antibiotics for possible anthrax exposure. Throughout the investigation the FBI interviewed more than 9,100 people and issued more than 6,000 subpoenas. Two people of interest were identified. One was eventually cleared and the other, Bruce Ivins, committed suicide before the investigation was complete. No arrests were ever made and no additional letters contaminated with anthrax have been found. On February 19, 2010, the Justice Department, FBI, and US Postal Inspection service announced that their investigation was complete and they named Ivins as the only suspect in the attacks. In the following years there were a number of reports that challenged the veracity of the FBI investigation and some scientists have questioned the conclusions that Ivins was solely responsible for the attacks. No new suspects have been identified and no new evidence has been made publicly available.50
Attacks and outbreaks involving biological agents are fortunately very rare. If and when they occur, they can be devastating to the people who are exposed and sickened and they can paralyze entire communities with fear. Responders will inevitably be on the front line of the response to incidents involving biological agents. We must be aware of the initial signs of an outbreak and take all available precautions to prevent contamination and limit the spread of the agent. Constant vigilance is needed and if we see something that is concerning then there must be a low threshold for reporting it. This course was designed to increase the student’s awareness of biological agents, their presentation, and the decontamination that is required for them. It is not a certification or credentialing program and if one intends to function as part of a specialized team that will respond to incidents involving biological agents, further training is needed.
Author Simon Taxel, Peer Reviewers James Schuetz, Lealand Raiford, et al.
Copyright CE Solutions. All Rights Reserved.
References: